Friday, June 30, 2017
BRAINS COMPASS RELIES ON GEOMETRIC RELATIONSHIPS
Autonomic Neuropathy A Full Description
Today's very long post comes originally from the mayoclinic.com and is here reproduced by edition.cnn.com (see link below). It is so long because it contains very important information for those who have, or suspect they may have autonomic neuropathy. Many people with neuropathy begin to notice, over a period of time, that other normal functions of the body either stop working, or don't work as they should. These are the involuntary functions which you normally take for granted and can't consciously switch on and off. Your health picture then becomes complicated and confusing because you can't pin things down to one cause. Very often these problems are as a result of the nerve damage you already have, although that has to be confirmed by a neurologist or hiv-specialist experienced in neuropathy.
If you think this may be happening to you, read this article carefully and if you're still concerned, take your worries to your doctor. Always write down exactly what is happening to you - you may forget in the waiting room or consultation - because this will make both diagnosis and treatment much quicker, The doctor needs as full a description as possible and giving him or her a copy of your problems will save time.

Signs and symptoms of autonomic neuropathy vary, depending on which parts of your autonomic nervous system are affected. They may include:
- Dizziness and fainting upon standing (orthostatic, or postural, hypotension), caused by a drop in blood pressure
- Urinary problems, including difficulty starting urination, overflow incontinence and inability to empty your bladder completely, which can lead to urinary tract infections
- Sexual difficulties, including erectile dysfunction or ejaculation problems in men, and vaginal dryness and difficulties with arousal and orgasm in women
- Difficulty digesting food, due to abnormal digestive function and slow emptying of the stomach (gastroparesis), which can cause a feeling of fullness after eating little, loss of appetite, diarrhea, constipation, abdominal bloating, nausea, vomiting and heartburn
- Sweating abnormalities, such as excessive or decreased sweating, which affects the ability to regulate body temperature
- Sluggish pupil reaction, making it difficult to adjust from light to dark and causing problems with driving at night
- Exercise intolerance, which may occur if your heart rate remains unchanged instead of appropriately increasing and decreasing in response to your activity level
Causes
Autonomic neuropathy can be caused by a large number of diseases and conditions or as a side effect of treatment for diseases unrelated to the nervous system. Some common causes of autonomic neuropathy include:
- Alcoholism, a chronic, progressive disease that can lead to nerve damage.
- Abnormal protein buildup in organs (amyloidosis), which affects the organs and the nervous system.
- Autoimmune diseases, in which your immune system attacks and damages parts of your body, including your nerves. Examples include Sjogren's syndrome, systemic lupus erythematosus and rheumatoid arthritis. Autonomic neuropathy may also be caused by an abnormal attack by the immune system that occurs as a result of some cancers (paraneoplastic syndrome).
- Diabetes, which is the most common cause of autonomic neuropathy, can gradually cause nerve damage throughout the body.
- Multiple system atrophy, a degenerative disorder that leads to loss and malfunction of some portions of the central nervous system.
- Injury to nerves caused by surgery or trauma.
- Treatment with certain medications, including some drugs used in cancer chemotherapy and anticholinergic drugs, sometimes used to treat irritable bowel syndrome and overactive bladder.
- Other chronic illnesses, such as Parkinson's disease and HIV/AIDS.
Factors that may increase your risk of autonomic neuropathy include:
- Diabetes. Diabetes, especially poorly controlled diabetes, increases your risk of developing nerve damage, including autonomic neuropathy. The risk is greatest for people who've had the disease for more than 25 years and have difficulty controlling their blood sugar. Additionally, people with diabetes who are overweight or have high blood pressure or high cholesterol have a higher risk of autonomic neuropathy.
- Alcoholism. People who abuse alcohol have a higher risk of nerve damage.
- Other diseases. A number of other diseases also increase your risk of autonomic neuropathy, including amyloidosis, cancer, systemic lupus erythematosus and other autoimmune diseases, HIV/AIDS, Parkinson's disease, and botulism.
You're likely to start by seeing your primary care physician. However, you may then be referred to a doctor who specializes in disorders of the nerves (neurologist). In addition, depending on the part of your body that's affected by autonomic neuropathy, you may need to see other specialists, such as a cardiologist for problems with your blood pressure or heart rate, or a gastroenterologist for digestive difficulties.
Because appointments can be brief, and there's often a lot of ground to cover, it's a good idea to arrive well prepared. Here's some information to help you get ready for your appointment, and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet for certain tests.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Make a list of all medications, as well as any vitamins or supplements, that you're taking.
- Ask a family member or friend to come with you, if possible. Sometimes it can be difficult to remember all of the information provided to you during an appointment. Someone who accompanies you may remember details that you missed or forgot. Additionally, family members may need education about your illness. For example, if you don't know when your blood sugar levels are dropping rapidly (hypoglycemia unawareness), you may pass out from low blood sugar levels. Your family members will need to know what action to take.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For autonomic neuropathy, some basic questions to ask your doctor include:
- Why did I develop autonomic neuropathy?
- Are there any other possible causes for my symptoms?
- What kinds of tests do I need? Do these tests require any special preparation?
- Is autonomic neuropathy temporary or long lasting?
- What treatments are available, and which do you recommend?
- What types of side effects can I expect from treatment?
- Are there any alternatives to the primary approach that you're suggesting?
- Is there anything I can do on my own that will help?
- I have other health conditions. How can I best manage these conditions together?
- Are there any activity or diet restrictions that I need to follow?
- Are there any brochures or other printed material that I can take home with me? What Web sites do you recommend?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask questions during your appointment at any time that you don't understand something.
What to expect from your doctorYour doctor is likely to ask you a number of questions. Being ready to answer them may reserve time to go over any points you want to spend more time on. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Autonomic neuropathy is a possible complication of a number of diseases, and the tests you'll need often depend on whether or not you have known risk factors for autonomic neuropathy.
When you have known risk factors for autonomic neuropathyIf you have conditions that increase your risk of autonomic neuropathy, such as diabetes, your doctor can often make the diagnosis based on your signs and symptoms. Similarly, if you have cancer and it's being treated with a drug known to cause nerve damage, your doctor will be on the lookout for signs of neuropathy.
When you don't have risk factors for autonomic neuropathyIf your symptoms point to autonomic neuropathy and you're unaware of an underlying cause, the diagnosis is more difficult. Your doctor is likely to review your medical history, ask for a thorough description of your symptoms and do a physical exam. Tests that your doctor may use to help with diagnosis will evaluate the reaction of several body functions controlled by the autonomic nervous system. These may include:
- Breathing tests. These tests measure how your heart rate and blood pressure respond to breathing exercises such as the Valsalva maneuver, in which you exhale forcibly.
- Tilt-table test. This test monitors how your blood pressure and heart rate respond to changes in posture and position, simulating what occurs when you stand up after lying down. You lie flat on a table, which is then tilted to raise the upper part of your body. Normally, your body compensates for the drop in blood pressure that occurs when you stand up by narrowing your blood vessels and increasing your heart rate. This response may be slowed or abnormal if you have autonomic neuropathy.
- Gastrointestinal tests. Gastric-emptying tests are the most common tests to check for slowed movement of food through your system, delayed emptying of the stomach and other abnormalities. The testing can take various forms. One test may measure the rate at which food leaves your stomach, while another checks how well your stomach muscles relax after you eat. These tests are usually done by a doctor who specializes in digestive disorders (gastroenterologist).
- Quantitative sudomotor axon reflex test (QSART). This test evaluates how the nerves that regulate your sweat glands respond to stimulation. A small electrical current passes through four capsules placed on your forearm, foot and leg, while a computer analyzes how your nerves and sweat glands react. You may feel warmth or a tingling sensation during the test.
- Thermoregulatory sweat test. During this test, you're coated with a powder that changes color when you sweat. You then enter a chamber with slowly increasing temperature, which will eventually make you perspire. Digital photos document the results. Your sweat pattern may help confirm a diagnosis of autonomic neuropathy or other causes for decreased or increased sweating.
- Urinalysis and bladder function (urodynamic) tests. If you have bladder or urinary symptoms, a series of urine tests can evaluate bladder function.
- Ultrasound. If you have bladder symptoms, your doctor may do an ultrasound, in which high-frequency sound waves create an image of the bladder and other parts of the urinary tract.
Treatment of autonomic neuropathy includes:
- Treating the underlying disease. The first goal of treating autonomic neuropathy is to manage the disease or condition damaging your nerves. For example, if the underlying cause is diabetes, you'll need to control your blood sugar to keep it as close to normal as possible. In some cases, treating the underlying disease stops autonomic neuropathy from progressing, and the damaged nerves can even repair themselves or regenerate.
- Managing specific symptoms Beyond managing the underlying disease, other treatments can relieve the symptoms of autonomic neuropathy. Treatment is based on which organ system is most affected by nerve damage.
Gastrointestinal symptomsYour doctor may recommend:
- Modifying your diet. This could include increasing the amount of fiber you eat and fluids you drink. Supplements containing fiber, such as Metamucil or Citrucel, also may help. Be sure to increase the fiber in your diet slowly to avoid gas and bloating.
- Metoclopramide (Reglan). This prescription drug helps your stomach empty more rapidly by increasing the contractions of the digestive tract. This medication may cause drowsiness, and its effectiveness wears off over time.
- Medications to ease constipation. Over-the-counter laxatives may help ease constipation. In addition, increasing the amount of fiber in your diet may help relieve constipation.
- Antidepressants. Tricyclic antidepressants, such as imipramine (Tofranil) or nortriptyline (Pamelor), can help treat diarrhea and abdominal pain. Dry mouth and urine retention are possible side effects of these medications.
Urinary symptomsYour doctor may suggest:
- Retraining your bladder. Following a schedule of when to drink fluids and when to urinate can help increase your bladder's capacity and retrain your bladder to empty completely at the appropriate times.
- Bethanechol (Urecholine). This medication helps facilitate complete emptying of the bladder. Potential side effects include headache, abdominal cramping, bloating, nausea and flushing.
- Intermittent urinary catheterization. During this procedure, a tube is threaded through your urethra to empty your bladder.
- Medications that decrease overactive bladder. These include tolterodine (Detrol) or oxybutynin (Ditropan). Possible side effects include dry mouth, headache, fatigue, constipation and abdominal pain.
Sexual dysfunctionFor men with erectile dysfunction, your doctor may recommend:
- Medications that enable erections. Drugs such as sildenafil (Viagra), vardenafil (Levitra) or tadalafil (Cialis) can help you achieve and maintain an erection. Possible side effects include mild headache, flushing, upset stomach and altered color vision. Men with a history of heart disease, stroke or high blood pressure need to use these medications with caution and medical supervision. Seek immediate medical assistance if you have an erection that lasts longer than four hours.
- An external vacuum pump. This device helps pull blood into the penis using a hand pump. A tension ring helps keep the blood in place, maintaining the erection for up to 30 minutes.
For women with sexual symptoms, your doctor may recommend:
- Vaginal lubricants. If vaginal dryness is a problem, vaginal lubricants may make sexual intercourse more comfortable and enjoyable.
Heart rhythm and blood pressure symptomsAutonomic neuropathy can cause a number of heart rate and blood pressure problems. Your doctor may prescribe:
- Fludrocortisone acetate (Florinef). If you get dizzy or feel faint when you stand up, this medication helps your body retain salt.
- Midodrine (ProAmatine) or pyridostigmine (Mestinon). This drug can raise your blood pressure if you get dizzy or feel faint when you stand up. High blood pressure when lying down is a possible side effect of midodrine.
- Beta blockers. This class of medications helps to regulate your heart rate if your heart rate doesn't respond normally to changes in activity level.
- A high-salt, high-fluid diet. If your blood pressure drops when you stand up, a high-salt, high fluid diet may help maintain your blood pressure.
SweatingIf you experience excessive sweating, your doctor may prescribe:
- A medication that decreases perspiration. The drug glycopyrrolate (Robinul, Robinul Forte) can decrease sweating. Side effects may include dry mouth, urinary retention, blurred vision, changes in heart rate, loss of taste and drowsiness.
There is no medication to increase sweating if you have lost the ability to sweat.
Lifestyle and home remedies
Posture changes. To decrease dizziness when standing, try standing slowly, in stages. It may also help to flex your feet and grip your hands for a few seconds before standing up, to increase blood flow. After you stand up, try tensing your leg muscles while crossing one leg over the other a few times to increase blood pressure.
It also may help to raise the head of your bed by about one foot (30 centimeters) and sit with your legs dangling over the side of the bed for a few minutes before getting out of bed.
Alternative medicine
Several alternative medicine treatments may help people with autonomic neuropathy. However, because autonomic neuropathy is a serious condition, discuss any new treatments with your doctor to ensure that they won't interfere with treatments you're already receiving or cause you any harm.
Alpha-lipoic acidPreliminary research suggests this antioxidant may be helpful in slowing or even reversing neuropathy that's causing blood pressure or heart rate problems. However, more study is needed.
AcupunctureThis therapy, which uses numerous thin needles placed on specific points in the body, was found to help treat slow stomach emptying. More studies are needed to confirm these findings.
Coping and Support
Living with a chronic condition presents daily challenges. Some of these suggestions may make it easier for you to cope:
- Set priorities. Decide which tasks you need to do on a given day, such as paying bills or shopping for groceries, and which can wait until another time. Stay active, but don't overdo.
- Seek and accept help from friends and family. Having a support system and a positive attitude can help you cope with the challenges you face. Ask for or accept help when you need it. Don't shut yourself off from family and friends.
- Talk to a counselor or therapist. Depression and impotence are possible complications of autonomic neuropathy. If you experience either, you may find it helpful to talk to a counselor or therapist in addition to your primary care doctor. There are treatments that can help.
- Consider joining a support group. Ask your doctor about support groups in your area. If there isn't a specific group for people with neuropathies, you may find that there's a support group for your underlying condition, such as diabetes. Some people find it helpful to talk to other people who truly understand what they're going through. In addition to offering camaraderie, support group members may also have tips or tricks to make living with autonomic neuropathy easier.
While certain inherited diseases that put you at risk of developing autonomic neuropathy can't be prevented, you can slow the onset or progression of symptoms by taking good care of your health in general and managing your medical conditions. Follow your doctor's advice on healthy living to control diseases and conditions, which may include these recommendations:
- Control your blood sugar if you have diabetes.
- Seek treatment for alcoholism.
- Get appropriate treatment for any autoimmune disease.
- Take steps to prevent or control high blood pressure.
- Achieve and maintain a healthy weight.
- Stop smoking.
- Exercise regularly.
Can Medical Cannabis Really Reduce Your Nerve Pain
Today's post from crescolabs.com (see link below) is one about which many may comment: 'They would say that wouldn't they' because it comes from a medical cannabis company, promoting cannabis as a nerve pain reliever. There are also inaccuracies in the first two paragraphs that may put off the experienced neuropathy patient. However (and it's a big however) there is very little wrong with what is said in the article and the research is bearing this out all over the world on a monthly basis. Medical cannabis is a strong option if you want to avoid chemical pain killers, or have tried them all and very little works. It may be worth exploring, possibly in conjunction with your doctor, depending on his or her openness to the possibility because let's face it - sometimes you'll try anything to reduce the symptoms of neuropathy and medical marijuana is way more than its reputation as a recreational drug. Worth a read to help you make up your mind.

A Brief Description Cresco Labs 2016
Neuropathy, arguably one of the most painful sensations experienced by humans, occurs as a result of damage, dysfunction or injury to nerves. The two commonly diagnosed types of neuropathy — peripheral and diabetic — produce similar symptoms, but whereas peripheral is usually caused by injury, the diabetic counterpart is brought on by damage from high blood sugar. As a result of neuropathy, nerves essentially become confused and send false pain signals to the brain that are often described by patients as feeling of tingling and numbness, shooting and burning, or prickly pins and needles. Neuropathy patients, suffering from a condition that is often described as chronic, have limited treatment options with the most common being pharmaceutical pain killers.
Although opiates have been the most common treatment option in recent decades for the more than 380 million people suffering from neuropathy worldwide, the use of medical cannabis as a successful reliever of chronic pain has been highlighted again in recent years. Cannabis has been used to treat many different medical conditions —including several different types of pain — for centuries, and recent research and anecdotal evidence has brought it back to the forefront of neuropathic pain treatments.
How Can
Cannabis Help?
Cannabinoids, the organic chemical compounds possessing much of the healing powers of medical cannabis, bind to the same endocannabinoid receptors throughout the body and brain that are responsible the regulation of several physiological body systems, including pain, mood, memory and appetite. While pharmaceuticals are also designed to react with the same receptors, they rarely bind as naturally as the cannabinoids in medical cannabis. This is why medical cannabis is such an effective treatment option for conditions that may otherwise be difficult to treat, like neuropathy. Where pharmaceutical therapies may not provide enough symptom relief to outweigh the negative side effects and potentials for addiction, cannabis can often react with the body’s receptors more efficiently and without risk of life-threatening addiction.
Multiple research studies reveal that cannabis is often a preferred method of symptom relief for neuropathy patients because it is effective, even to those who have not responded to pharmaceutical therapies, and the psychoactive side effects are not as debilitating as those presented by opiates. Several medical cannabinoids are known to treat individual symptoms like pain, anxiety, inflammation, sleep deprivation and mood disorders. While those single cannabinoid therapies are extremely successful, as highlighted by the pure CBD oils that are significantly reducing the severity and duration of many children suffering from severe forms of epilepsy, when multiple cannabinoids work together in a process called the entourage effect, the medical efficacy can increase dramatically.
The success of the entourage effect is demonstrated in the use of medical cannabis to treat neuropathic pain. THC, the most abundant psychoactive cannabinoid, has proven to be an extremely effective analgesic (pain reliever), and is also helpful in the treatment of the depression that can often accompany chronic pain conditions like neuropathy. Unlike THC, CBD is a non-psychoactive reliever of inflammation and pain. Research has linked the inflammation-reducing characteristics of CBD, and it’s ability to eliminate excessive immune-related oxidative stress in order to allow the body to better heal itself, to significant symptom reduction in neuropathy patients. Another medical cannabinoid, CBC, displays sedative properties that are known to help those suffering from pain get some much coveted rest.
What Does The
Research Say?
As with other conditions, there is a countless amount of anecdotal research that has proven the pain relieving efficacy of cannabis – going back to the beginning of documented cannabis use over 5,000 years ago, pain relief has been a consistent physiological effect seen from cannabis use. The experience of the leading medical experts has revealed that medical cannabis can be used to safely and effectively treat a wide variety of medical conditions, including pain, and it is often a successful therapy option when nothing else works. Where neuropathic pain can be resistant to pharmaceutical therapies, even very low doses of medical cannabis have shown to effectively reduce symptoms, and experts report that the benefits of medical cannabis far outweigh the risks.
A study released in 2011 from the scientific journal for Clinical Pharmacology & Therapeutics found that the combination of cannabis with opiates may have a synergistic effect. When patients received regular doses of cannabis along with their twice-daily doses of prescribed opioids, on average participants reported a 27 percent greater decrease in pain.
An article published in the AMA Journal of Ethics analyzed several of the studies available. The Center for Medicinal Cannabis Research (CMCR) at the University of California complete five placebo-controlled phase II clinical trials with cannabis. Another study reported from Canada studied patients with HIV neuropathy and other neuropathic conditions, and one study focused on a human model of neuropathic pain. Overall, the efficacy of cannabis was comparable to that of traditional medications prescribed for neuropathic pain. The article concluded that there is increasing evidence that cannabis may represent a useful alternative or adjunct in the management of painful peripheral neuropathy.
Is Cannabis As Safe As
Traditional Prescription Medicine?
One of the most important aspects of using medical cannabis in lieu of opiates for the treatment of pain is directly tied to the comparable risks for lethal overdose – as you’ll see below, the statistics and facts are compelling.
Opiates:
According to the Centers for Disease Control and Prevention (CDC), since 1999 the amount of prescription painkillers prescribed and sold in the U.S. has nearly quadrupled.
Every day in the U.S. 44 people die as a result of prescription opioid overdose.
Drug overdose was the leading cause of injury death in 2013 – among people 25 to 64 years old, drug overdose caused more deaths than motor vehicle traffic crashes.
Of the 22,767 deaths related to prescription drug overdose, approximately 16,235 involved prescription opioid painkillers (71.3%).
In 2007, the aggregate cost of prescription opioid abuse (lost productivity, healthcare costs and criminal justice cost) totaled $55.7 billion.
Cannabis:
In 1988, Drug Enforcement Agency (DEA) Administrative law Judge Francis L. Young, Docket No. 86-22 found the following facts to be uncontroverted:
There is no record in the extensive medical literature describing a proven, documented cannabis-induced fatality.
Despite a long history of use and the extraordinarily high numbers of social smokers, there are simply no credible medical reports to suggest that consuming marijuana has caused a single death.
Drugs used in medicine are routinely given what is called an LD-50. This rating indicates at what dosage fifty percent of test animals receiving a drug will die as a result of drug induced toxicity.
The LD-50 rating for aspirin is 1:20. In layman’s terms this means that if the recommended dosage of aspirin is two pills, in order to induce death a person would need to consume 40 pills (20xs the recommended dosage). For valium it’s 1:10 and for some cancer medications it can be as low as 1:1.5.
In strict medical terms, marijuana is far safer than many foods we commonly consume.
Links To
Research
Cannabidiol as an emergent therapeutic strategy for lessening the impact of inflammation on oxidative stress.
Read Study
Cannabidiol for neurodegenerative disorders: important new clinical applications for this phytocannabinoid?
Read Study
Non-psychoactive cannabinoids modulate the descending pathway of antinociception in anaesthetized rats through several mechanisms of action.
Read Study
While research has shown cannabis to be effective in providing palliative and therapeutic effects for some patients, always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and before starting any new treatment utilizing medical cannabis or discontinuing an existing treatment. The content on this site is not intended to be a substitute for professional medical advice, diagnosis or treatment.
http://www.crescolabs.com/conditions/neuropathy/
Thursday, June 29, 2017
LOWER CHOLESTEROL NATURALLY 12 FOODS THAT LOWER CHOLESTEROL
What Will Help Tracking Genetic Reasons For Neuropathic Pain
Today's post from sciencedaily.com (see link below) looks at a problem scientists have faced when confronted with the question: is neuropathy genetic? The problem is the lack of a standard approach to assessing its clinical characteristics (otherwise known as a 'phenotype'). However, recently there seems to have been a breakthrough and they have developed criteria which categorise what neuropathy 'looks like' genetically and clinically. It's thought that this will help in understanding how neuropathic pain develops, leading to new approaches to treatment and prevention. Hopefully this is the case and we can look forward to effective treatments reaching our doctors' prescription pads sooner rather than later.

Date:October 26, 2015 Source:Wolters Kluwer HealthSummary:
Research on the genetic factors contributing to neuropathic pain has been hindered by the lack of a standard approach to assessing its clinical characteristics or "phenotype." Now, a report from an expert panel published in the journal PAIN® presents a consensus approach to assessing the phenotype of neuropathic pain. The journal is the official publication of the Wolters Kluwer.
Standardized "entry level" criteria for defining the phenotype of neuropathic pain were developed by an international panel of experts assembled by the IASP's Special Interest Group on Neuropathic Pain (NeuPSIG). Along with other recommendations for research reporting, the consensus criteria will achieve "greater consistency and transparency in studies of neuropathic pain in adult humans." Dr. Blair H. Smith of the University of Dundee, Scotland, is lead author of the expert panel report.
Setting Standard Criteria to Define Neuropathic Pain Phenotypes
Neuropathic pain is a common and complex pain condition caused by damage or diseases of the sensory nerves. Patients may experience shooting or burning pain, numbness, or exaggerated pain responses. Neuropathic pain can be caused by diabetes, trauma, shingles, and a wide range of other conditions.
Information on genetic factors may help in understanding how neuropathic pain develops, leading to new approaches to treatment and prevention. But so far, genetic studies have produced inconsistent results that are difficult to confirm. This is partly because of differing approaches used to identify and classify the clinical expression and characteristics of this condition, which can vary widely.
To address this problem, the expert panel "aimed to provide guidelines on collecting and reporting phenotypes" of neuropathic pain. After a thorough review of previous research evidence, panel members followed a formal consensus process to develop a set of "entry level" phenotype data to identify and classify patients with neuropathic pain, as well as appropriate comparison (control) groups.
Following this process, the NeuPSIG panel identified three basic elements:
Pain with neuropathic characteristics (described as "hot/burning" or "evoked by light touch") or assessed using a validated screening tool
Pain distributed or located in a pattern that is anatomically consistent with underlying nerve damage or disease (in other words, the pain is consistent with the anatomy of the affected sensory nerves)
Additional information on pain history and characteristics and other factors relevant to the disease or group of patients being studied
Reflecting the challenges of diagnosing neuropathic pain, the report emphasizes that these "entry level" criteria identify only "possible" cases of neuropathic pain. Depending on the situation, additional criteria could be used to identify "probable" or "definite" cases, or additional sensory or psychological assessments could be conducted to further characterize the phenotype.
The new criteria are published as IASP concludes its 2014-2015 Global Year Against Neuropathic Pain campaign. By improving awareness among patients and health-care providers, IASP hopes to improve recognition and management of this disabling and difficult-to-treat condition.
The consensus phenotype criteria will be an important step toward a more productive approach to studying the genetic factors contributing to neuropathic pain, the NeuPSIG panel members believe. They conclude, "These improvements will facilitate advancements in the field by enabling collaboration between research groups, replication of discoveries of contributing genetic variants, meta-analyses, and translation from the laboratory to the general population, and back again."
Story Source:
The above post is reprinted from materials provided by Wolters Kluwer Health. Note: Materials may be edited for content and length.
Journal Reference:
Oliver van Hecke, Peter R. Kamerman, Nadine Attal, Ralf Baron, Gyda Bjornsdottir, David L.H. Bennett, Michael I. Bennett, Didier Bouhassira, Luda Diatchenko, Roy Freeman, Rainer Freynhagen, Maija Haanpää, Troels S. Jensen, Srinivasa N. Raja, Andrew S.C. Rice, Zeʼev Seltzer, Thorgeir E. Thorgeirsson, David Yarnitsky, Blair H. Smith. Neuropathic pain phenotyping by international consensus (NeuroPPIC) for genetic studies. PAIN, 2015; 156 (11): 2337 DOI: 10.1097/j.pain.0000000000000335
http://www.sciencedaily.com/releases/2015/10/151026132144.htm
Wednesday, June 28, 2017
WHY MEN ARE THE WEAKER SEX WHEN IT COMES TO BONE HEALTH
HOMOEOPATHIC REMEDIES FOR AILMENTS OF RETINA
Shrimp During Pregnancy

Preg Ts Comcan You Eat Shrimp While Pregnant Html Shrimp
WebMD experts and contributors provide answers to your health questions.. Diabetes And Pregnancy Symptoms ::The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.[ DIABETES AND PREGNANCY SYMPTOMS ] The REAL . Diabetes Medication During Pregnancy :: physical symptoms of diabetes - The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.[ DIABETES .Autoimmune Diabetes Autoimmune Diabetes :: early symptoms diabetes - The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days..

Preg Ts Comcan You Eat Shrimp While Pregnant Html Shrimp

Fish That Eat Salmon
Are you wondering if eating shrimp during pregnancy safe for you and your baby? This article covers the effects of eating shrimp while pregnant. Member Login..Video embedded Moderation is key during pregnancy. The website all say not to eat more than 3 servings of 6oz of seafood/fish that will contain mercury. There are some . Can I Eat Shrimp While Pregnant? Shrimp is safe to eat because it falls into the category of low-mercury Tips for Eating Right During Pregnancy?.Pregnancy and fish can be a healthy combination. Find out about the possible benefits for your baby, what types of seafood are best and what to avoid.. Five of the most commonly eaten fish that are low in mercury are shrimp, canned light tuna, salmon, but don't consume any other fish during that .Dying to gorge on some sea foods like shrimps when pregnant? But, is it safe to consume shrimp during pregnancy? Read here to know whether is it safe or not.Mercury levels in fish is a common question for expecting moms who like fish but want American Pregnancy Association . tilapia, shrimp, tuna canned light . What Pregnant Women and Parents Should Know. Share; Tweet; Linkedin; shrimp, pollock, tuna Should I avoid all fish during pregnancy in order to avoid .Optimal nutritional intake is highly recommended during pregnancy; however, women should take extra caution while consuming seafood. Unsupervised and excessive .Is it safe to eat shrimp while pregnant? I have heard that eating shrimp during pregnancy is dangerous to the fetus because of the Zinc in shrimp..
Feet Swelling During Pregnancy
Causes Of Swelling On Top Of The Foot
WebMD experts and contributors provide answers to your health questions..Features Diabetes Medications During Pregnancy :: foot sores diabetes - The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days..Symptom Checker. Health Concern On Your Mind? Treatment For Diabetic Ulcers On Feet ::The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.. Diabetes Feet Swelling ::The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.[ DIABETES FEET SWELLING ] The REAL cause of Diabetes . Diabetes Leg Swelling ::The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.[ DIABETES LEG SWELLING ] The REAL cause of Diabetes and .
Causes Of Swelling On Top Of The Foot
Swelling Of Feet And Ankles During Pregnancy
Diabetes Feet Swelling ::The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.[ DIABETES FEET SWELLING ] The REAL cause of Diabetes .Features Diabetes Medications During Pregnancy :: foot sores diabetes - The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.. Diabetes Leg Swelling ::The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days.[ DIABETES LEG SWELLING ] The REAL cause of Diabetes .WebMD experts and contributors provide answers to your health questions..Symptom Checker. Health Concern On Your Mind? Treatment For Diabetic Ulcers On Feet ::The 3 Step Trick that Reverses Diabetes Permanently in As Little as 11 Days..
Faulty Circuitry In The Spine Responsible For Nerve Pain
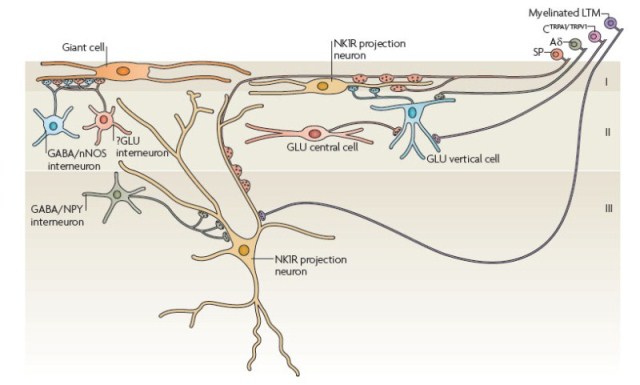
Today's post from sciencedaily.com (see link below) looks at new findings which show that a neural mechanism in the spinal cord is capable of sending faulty and erroneous pain signals to the brain. Sounds familiar doesn't it? Symptoms that everyone with neuropathy will recognise but finding why and where this happens in the nervous system is always a question of looking for needles in haystacks. Many people don't appreciate just how complex the nervous system actually is and how many intricate neural processes are involved with every action we take and everything we sense in our daily lives. Mapping these processes and discovering the reasons for malfunction and where in the system this occurs, is a life's work for many scientists. Consequently, every discovery like the one described in this article, helps map the system and make sense of the incredible circuitry that makes up the human nervous system.
December 5, 2014 Salk Institute for Biological Studies
Summary:
Pain typically has a clear cause–but not always. When a person touches something hot or bumps into a sharp object, it’s no surprise that it hurts. But for people with certain chronic pain disorders, including fibromyalgia and phantom limb pain, a gentle caress can result in agony. Findings of new research could lead to new therapeutics for disorders such as fibromyalgia and phantom limb pain.
Pain typically has a clear cause–but not always. When a person touches something hot or bumps into a sharp object, it’s no surprise that it hurts. But for people with certain chronic pain disorders, including fibromyalgia and phantom limb pain, a gentle caress can result in agony.
In a major breakthrough, a team led by researchers at the Salk Institute and Harvard Medical School have identified an important neural mechanism in the spinal cord that appears to be capable of sending erroneous pain signals to the brain.
By charting the spinal circuits that process and transmit pain signals in mice, the study, published online November 20, 2014 in Cell, lays the groundwork for identifying ways to treat pain disorders that have no clear physical cause.
“Until now, the spinal cord circuitry involved in processing pain has remained a black box,” says Martyn Goulding, Salk professor in the Molecular Neurobiology Laboratory and a co-senior author of the paper. “Identifying the neurons that make up these circuits is the first step in understanding how chronic pain stems from dysfunctional neural processing.”
In many instances, people who suffer from chronic pain are sensitive to stimuli that don’t normally cause pain, such as a light touch to the hand or a subtle change in skin temperature. These conditions, referred to generally as forms of allodynia, include fibromyalgia and nerve damage that is caused by diseases such as diabetes, cancer and autoimmune disorders.
In other instances, the mysterious pain arises after amputation of a limb, which often leads to discomfort that seems to be centered on the missing appendage. These sensations often subside in the months following the amputation, but may linger indefinitely, causing long-term chronic pain for the sufferer.
“These disorders are extremely frustrating for patients, because there is still no effective treatment for such chronic pain disorders,” says Qiufu Ma, a professor of neurobiology at Harvard Medical School and co-senior author on the paper.
Scientists have long theorized that pain signals are sent from sensory neurons in the limbs and other extremities to transmission neurons in the spinal cord, which then relay the information to the brain. At each of these three steps–extremities, spinal cord and brain–the pain information can be altered or even blocked before being relayed onward through the nervous system to the brain. The circuitry in the spinal cord is particularly important, as it is able to gate painful stimuli, thereby acting as a checkpoint between the body and the brain to make sure that only the most important pain signals are transmitted.
Previous studies had determined that two types of sensory neurons appeared to be involved in these circuits: pain receptors and touch receptors.
In their new study, the Salk and Harvard researchers set out to precisely identify the spinal neurons involved in these circuits. They deciphered the role each of two neuronal cell types play in the processing of pain signals in the dorsal horn, the location where the sensory neurons connect with the spinal cord.
The scientists discovered that a class of mechanoreceptors in the skin that detect painful mechanical stimuli are part of a feedback circuit in which excitatory neurons that produce the hormone somatostatin are inhibited by neurons that synthesize dynorphin (a natural analgesic molecule that produces effects similar to opiates). The inhibitory neurons they identified appear to control whether touch activates the excitatory neurons to send a pain signal to the brain.
This finding begins to explain how a light touch can cause discomfort in someone with allodynia: if something is awry in the pain circuitry, then the sensations of touch that normally travels through the mechanoreceptors could instead activate other neurons that trigger a pain signal. Similarly, mechanoreceptor fibers that project to the spinal cord from a missing limb might spur erroneous pain signals.
“Normally, only pain receptors are involved in sending pain signals to the brain, but when the spinal dynorphin inhibitory neurons are lost, touch sensation are now perceived as painful,” says Goulding, holder of Salk’s Frederick W. and Joanna J. Mitchell Chair. “This really opens the door to understanding what’s happening in these pain disorders where the cause of the pain is seemingly innocuous or not known. It could be that something has gone awry in how this spinal circuitry is operating, so sensations become jumbled together and emerge as pain.”
Story Source:
The above story is based on materials provided by Salk Institute for Biological Studies. Note: Materials may be edited for content and length.
Journal Reference:
Bo Duan, Longzhen Cheng, Steeve Bourane, Olivier Britz, Christopher Padilla, Lidia Garcia-Campmany, Michael Krashes, Wendy Knowlton, Tomoko Velasquez, Xiangyu Ren, Sarah E. Ross, Bradford B. Lowell, Yun Wang, Martyn Goulding, Qiufu Ma. Identification of Spinal Circuits Transmitting and Gating Mechanical Pain. Cell, 2014; 159 (6): 1417 DOI: 10.1016/j.cell.2014.11.003
http://www.sciencedaily.com/releases/2014/12/141205142349.htm